Scoliosis; Types, Assessment and Treatment
Types, Cause, Examination and Treatment
The term Scoliosis is a condition first described in detail by the Greek physician Hippocrates who took its name from the Greek word 'scolios' meaning 'crooked' (5). A scoliosis is normally considered if there is at least ten degrees of spinal angulation with lateral curvature shown on a posterior-anterior radiograph (4).
Scoliosis is the most common deformity of the spine with a direct effect on the thoracic cage and often consists of lateral displacement with associated rotation of the vertebrae (5).
As the UK Scoliosis Association highlights, scoliosis is not a disease or contagious and 3 to 4 children per 1000 may require supervision (8).
Scoliosis can develop at any age but usually becomes most clinically evident during growth, growth spurts or rapid somatic growth (5). The condition can be classified broadly as congenital, neuromuscular, syndrome-related, idiopathic and spinal curvature due to secondary reasons (4).
Idiopathic scoliosis is the most common type and approximately accounts for 80% of scoliosis cases. Congenital scoliosis is caused by structural abnormalities of bone and neural tissues and is the second most common type and accounts for approximately 10% of cases (7). Neuromuscular, developmental, and tumor-associated scoliosis altogether constitute the remaining 10% . Currently, degenerative scoliosis and traumatic scoliosis are also considered important subcategories by those involved in management of the disease (7).
Scoliosis is usually classified as primary (i.e. idiopathic) or secondary. Idiopathic scoliosis is
further classified according to the patient’s age,
whereas secondary scoliosis is classified
according to the cause.
- Infantile
- Young children (early onset)
- Older children (adolescent idiopathic)
- Adults (degenerative or de novo)
A scoliosis is classified with accordance to the side of its occurence into either left or right sided curves.Classification of scoliosis is dependent upon which region of the spine is affected and usually termed 'thorcaic', 'lumbar' or 'thoracolumbar'. The involvement of any of these areas is significant as organ function will need to be taken into consideration. For instance, the thoracic spine is primarily responsible for the respiratory and cardiovascular complications of scoliosis (4, 5). A lumbar spine scoliotic pattern can later affect an individual's pelvic floor strength, incontinence or can lead to bowel and bladder related disorder(s) (6).
It has been postulated that the condition might be related to proprioception or homeostasis disorders along with inheritance or genetics as well as metabolic, hormonal and biomechanical factors(1). It is worth noting that biomechanical or hormonal disturbances can cause reduced vertebral bone mass which can further progress spinal curvature (2).
Dextroscoliosis and Levoscoliosis
Dextroscoliosis
is abnormal sideways curvature of the spine laterally displaced to the right and also known as a dextrocurvature
(6) .
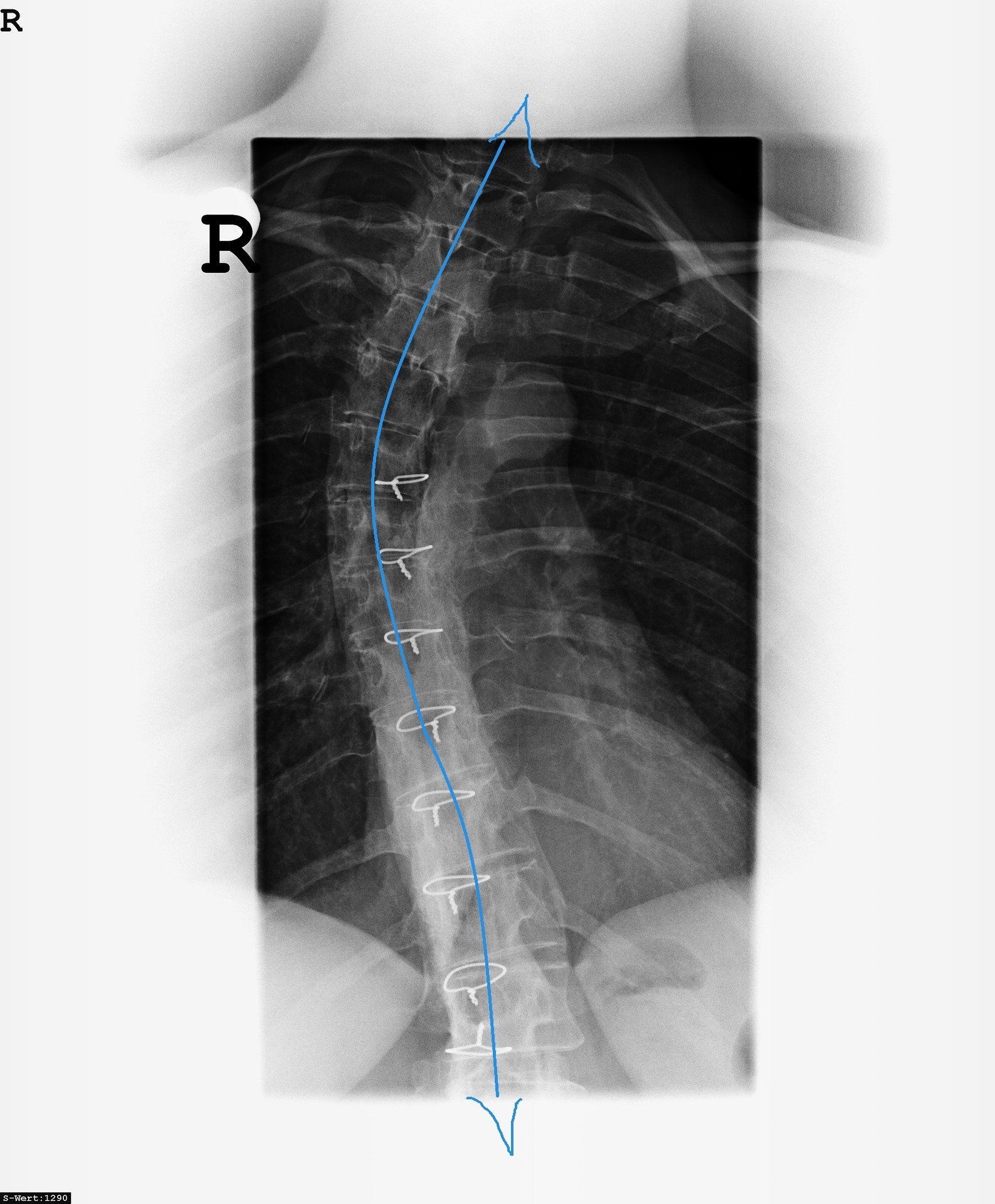
The above picture (Figure 1) shows a lumbar dextroscoliosis
which characterises an S-shaped curvature of the spine, specifically the lower back region.
Thoracic dextroscoliosis
is an abnormal curvature within the thoracic region of the spine that also curves laterally to the right.
When a spinal curve deviates to the left, it is known as levoscoliosis
or levocurvature
. A levoscoliosis can affect either the lumbar or thoracic regions of the spine and known as a thoracic levoscoliosis
and lumbar levoscoliosis
respectively (10).
Structural or Non Strucutral Scoliosis
Structural:
Scoliosis may be structural
which is when the patient's spine has an anatomical physical curve that can be observed whilst the patient is standing or sitting.
Structural scoliosis can be idiopathic which tends to affect girls more than boys during adolescence. A UK study showed that scoliosis in girls over 8 years of age out numbered boys by almost 3 to 1 (4). Idiopathic scoliosis can be further classified into infantile, juvenille and adolescent types or early and late onset (4).
Structural scoliosis can also be secondary to congenital or neurological disorders (e.g. cerebral palsy or paralysis), neuromuscular conditions, (e.g. Duchenne muscular dystrophy), tumours, trauma or syndromic conditions (e.g. Marafans syndrome and neurofibromatosis) (4, 5).
Non Structural:
Also known as a functional scoliosis with the latter to be caused from conditions such as lower limb disorders such as limb length discrepancy, herniated discs, hip dysplasia or limb deficiency syndromes.
The Nature of Scoliosis
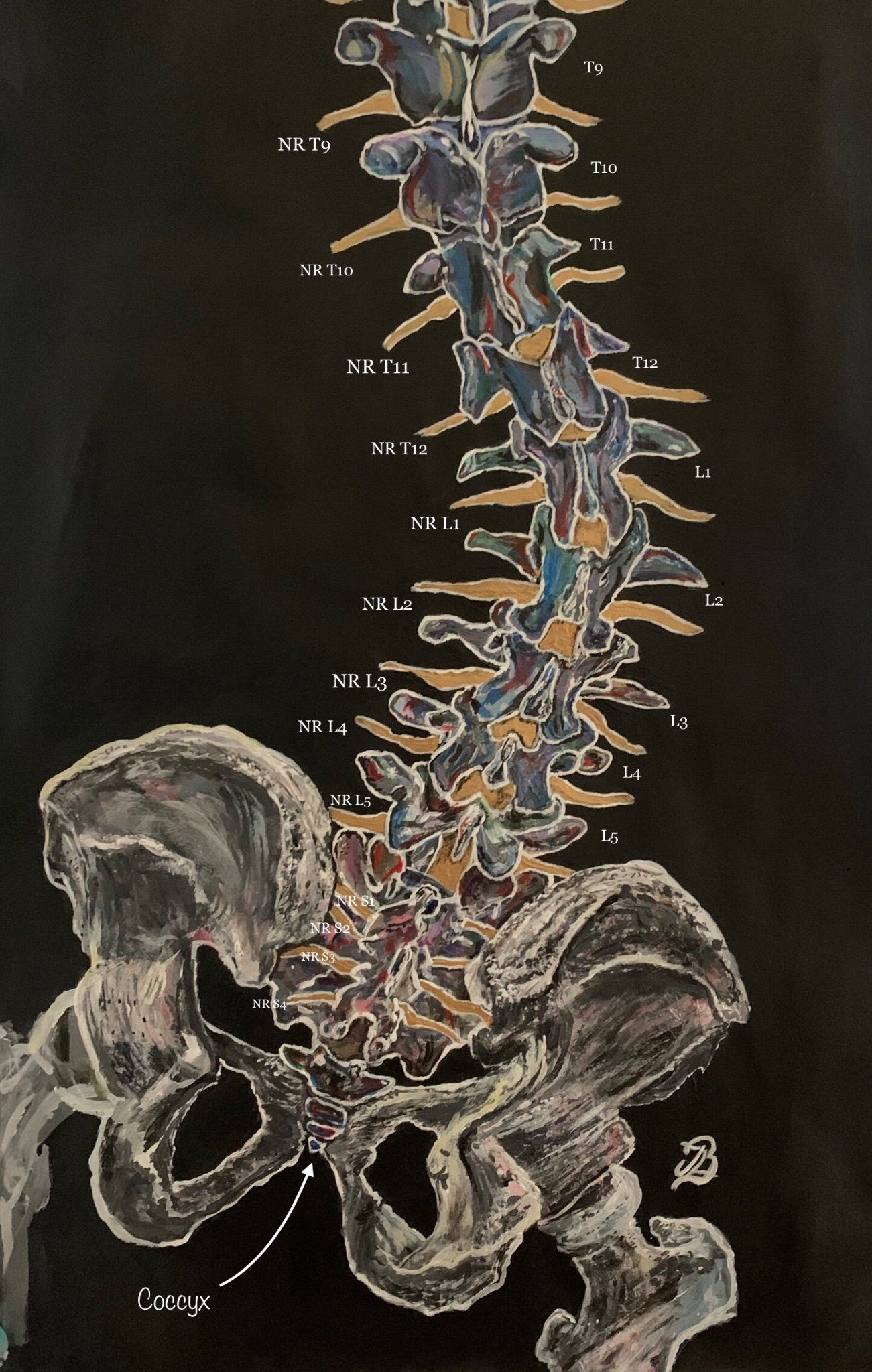
Each curve of a scoliosis is classified as either having a convex or concave side as well as a primary and a secondary curve (5). The primary curve is usually stiffer and the curve site is classified with accordance to the location of the apical or apex vertebra in the coronal plane within either cervical, thoracic or lumbar spine (5).
The apical vertebra is the most rotated vertebra in the curve and the end vertebrae are the most cephalad and caudal whose superior and inferior surfaces have the most maximal tilt towards the concavity of the spinal (either concave or convexed) curve.
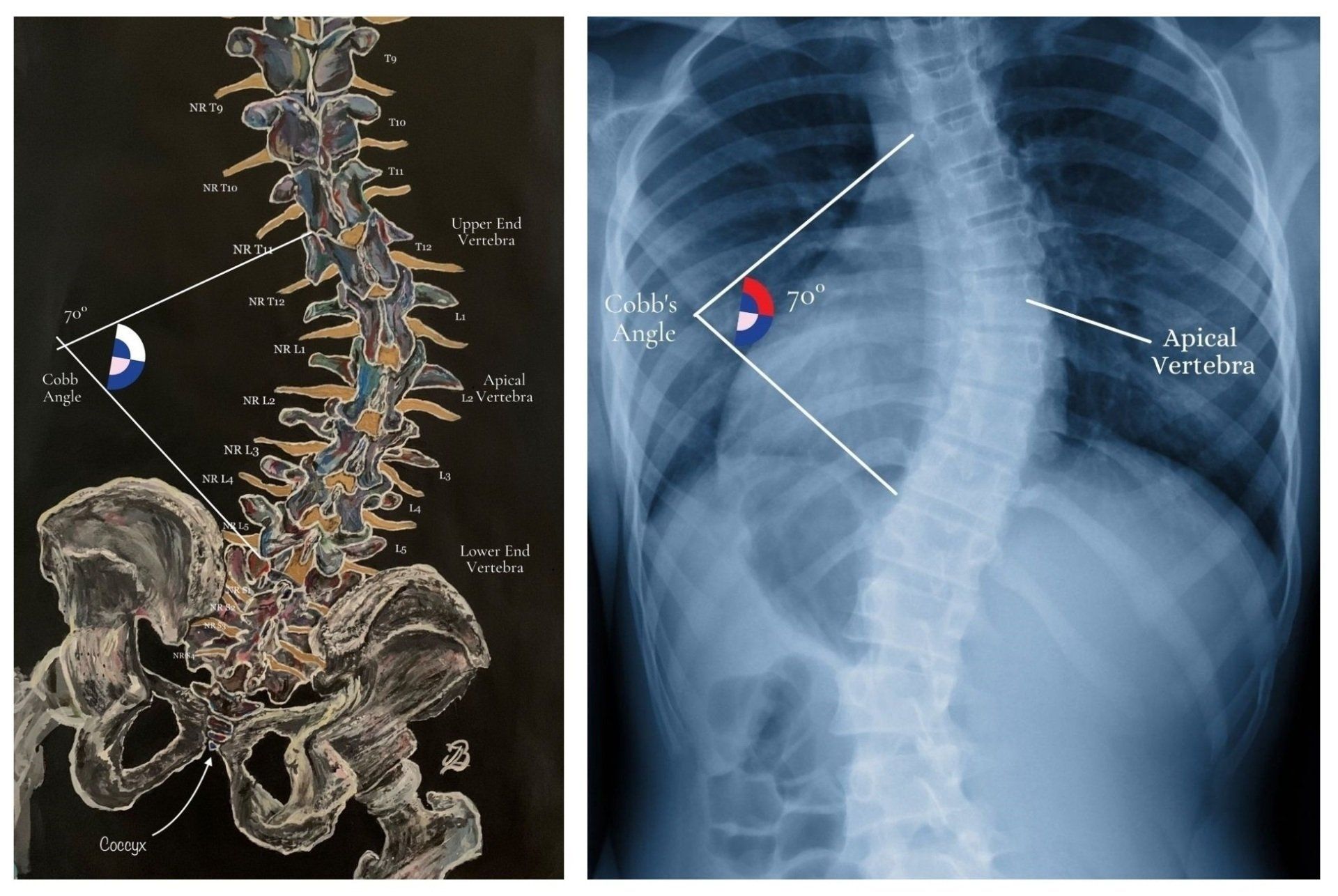
Cobb's Angle
The Cobb angle is useful for assessing initial stages of a scoliotic curve, whether there is an increasing magnitude and helps one to decide when or if it is appropriate to operate (4). The size of the curve within a scoliosis is assessed via the measurement of the cobb angle. Here, lines are drawn perpendicular to the transverse axes containing the upper and lower end vertebraeand where the lines intersect is the cobb angle. The angle can now be measured using specialised computer software.
Adolescent and Infantile Scoloisis
Infantile and juvenile idiopathic curves: infantile and Juvenile
are terms used to describe curves that develop from ages 0 to 3
years and 4 to 10 years of age respectively. More recently the term “early
onset’ has been used to classify curves that develop before the
age of 10 years (5).
Although not (yet) proven, the rate or severity of scoliosis between boys and girls during pubertal stages might be associated with hormonal factors (in particular growth hormone) (7).
In the 1980's, adolescent idiopathic curves have been classified by King and Moe who found that there are five distinct curve patternsbased on standing radiographs of the spine. The aim of
this system was to determine a reliable method for selecting vertebrae for fusion. The curve types were stratified from I-V with type II and
III being most common. Type II is a thoracolumbar curve
while Type III is a thoracic curve. There is poor intra/inter
observer reliability with this system. It also only assesses the
curve in the coronal plane, does not address lumbar/thoracolumbar/double major/triple major curves and does not
consider the 3-dimensional scope of the deformity (5).
Neuromuscular Scoliosis
As Koumbourlis (2006) highlights, neuromuscular scoliosis differs to idiopathic scoliosis. In idiopathic scoliosis, respiratory muscle dysfunction results to distortion of
the thoracic cage. In neuromuscular scoliosis, the thoracic
cage is distorted because of the underlying muscle weakness. Various neuromuscular disorders
are clinically evident during early infancy with distortions observed within the thorax which can be severe (7). During this period of
rapid lung growth and development, this can also cause severe
impairment of the lung growth.
Further differentiation between the two types is that idiopathic scoliosis tends to
stabilise (or progress at a lower rate) after the
person reaches skeletal maturity.
However, neuromuscular scoliosis progressively worsens from the muscle weakness and complications are potentially greater because of problems such as chronic, recurrent aspiration pneumonia secondary to impaired clearance of airway
secretions (7).
Some syndromes where scoliosis is likely to happen are connective tissue disorders (Marfan’s and Ehlers-Danlos syndrome), trisomy 21, Prada-Willi, Retts syndrome and Beale’s syndrome. Duchenne muscular dystrophy or spinal muscular atrophy can prevent or severely reduce muscle activation thus encouraging the development of muscle imbalance, muscle atrophy and the progression of a spinal scoliotic curvature (7).
Patients with these conditions often develop scoliosis or kyphosis, or both. As they grow and their trunk muscles become weaker, the spine gradually begins to collapse, which creates a long, C-shaped collapsing scoliosis.
For children who use a wheelchair, progressive curves can make it difficult for them to sit comfortably. Large curves (measuring 80 degrees or above) in the upper or middle parts of the spine may cause lung problems (8, 9).
Interestingly, the association of scoliosis with conditions known to be related to collagen abnormalities (e.g. Marfan syndrome) can be corroborated by the abnormalities in the amount of collagen associated with low glycosaminoglycan levels in the apical discs (7).Signs and Symptoms
In the majority of cases, pain is not usually a reason for patients to seek further medical assistance but may present with either back or rib prominence pain (Haleem and Nnadi, 2018). Night is pain is an unusual complaint and should be referred for further imaging to rule out spinal tumour.
Other important features to keep in mind are
balance and gait disturbance, bowel and bladder control or lack
of and any other neurological deficit. These should alert the
examiner to look for other pathological causes including tumours
(both intra and extradural) and other central causes (e.g.
syringomyelia) (5,7).
Curve progression needs to be carefully monitored. The risk of
curve progression depends on timing of growth spurts and also
on the amount of growth remaining in each individual patient. In
younger children (particularly those less than 10 years of age lung volume growth may be impaired and untreated severe or
progressive scoliosis can lead to or worsen chronic restrictive
respiratory disease.
Chiari malformations, Syringomyelia and spinal cord tethering are important
associations with congenital and Early Onset scoliosis.
Treatment
Treatment for scoliosis is based on the type of scoliosis, magnitude of the curve, number of years of
growth remaining and the patient’s opinion about the shape
of their back (5,7).The trunk deformity and
balance is also included in the decision-making process(5) report, the management and treatment of patients with either congenital,
neuromuscular, syndrome-associated or idiopathic scoliosis younger than 10 years of age presents a number of controversies.
The treatment options for AIS include observation,
bracing and surgery. While many other factors must be considered, the general goal is to keep curves under 50° during maturity.
Observation
Typically, observation is recommended for
immature patients with curves of less than 25°.The most reliable method of monitoring
growth is simple height measurements. Therefore, the primary physician often possesses this information from their
annual examinations
Braces
Compliance and wearing time of braces seem to have a role in the effectiveness of bracing and although they do not permanently improve or correct spinal curves, they do try to prevent it from worsening (5). Braces include the Milwaukee brace, Boston brace
and the Charleston bending brace (5,7).
Surgery
Surgery is usually performed during adolescence, but newer techniques have allowed good correction to be
accomplished into early adulthood (5, 7).Surgical correction of idiopathic scoliosis is considered for
curves greater than 45° in immature patients and for curves
greater than 50° in mature patients.The goals for surgical
treatment include prevention of progression, improve spinal
alignment and balance and help improve alignment between hips and shoulders and the head over the sacrum (5, 7).The spine is corrected with a combination of rods, hooks, screws and wires while being fused by
bone graft – either from the patient, a cadaver or artificiallyThe techniques for the correction and fusion change
quickly; long-term results have not been obtained for the
newest techniques. However, with older technology, good
results have been found in a 20-year follow-up period (5,7).
How Might Ostoepathy Be Able To Help?
Once a clinical assessment has been performed by the practitioner, Osteopathy treatment may involve a wide range of different techniques and management will depend on the individual's case. Everybody is uniquely different and spinal curves will differ to each individual person.
One example of treatment management that might be chosen to apply are gentle joint mobilisation techniques for the thoracic and lumbar spine, pelvis and rib cage with the aim of increasing their joint range of movement. Soft tissue massage techniques and passive stretching might also be applied with the aim of reducing tension and compression within the associated shortened muscles and reduce pressures within the joints. Home exercises for patients are often advised to be performed.
References
1. Choudhry, M. N., Ahmad, Z., Verma, R. (2016) Adolescent Idiopathic Scoliosis,
The
Open Orthopaedics Journal, 10: 143-154.
https://openorthopaedicsjournal.com/contents/volumes/V10/TOORTHJ-10-143/TOORTHJ-10-143.pdf
2. Fadzan, M., Bettany-Saltikov, J. (2017) Etiological Theories of Adolescent Idiopathic Scoliosis: Past and Present, The Open Orthopaedics Journal, 11: pp. 1466-1489.
https://openorthopaedicsjournal.com/contents/volumes/V11/TOORTHJ-11-1466/TOORTHJ-11-1466.pdf
3. Francis, M. J. O., Sanderson, M. C., Smith, R. (1976) Skin Collagen in Idiopathic Adolescent Scoliosis and Marfan's Syndrome, Clinical Science and Molecular Medicine; 51: 467-474.
4. Haleem, S., Nnadi, C. (2018) Scoliosis: A Review, Paediatrics and Child Health ; 28: 5; 2019 – 217.
5. Janicki, J. A., Alman, B. (2017) Scoliosis: Review of diagnosis and Treatment; Orthopaedic Subseciality Article , 12; 9: 771 – 776.
6. Kim, H., Kim, H. S., Moon, E. S., Yoon, C-S., Chung, T-S., Song, H-T., Suh, J-S., Lee, Y, H., Kim, S., (2010)S coliosis Imaging: What Radiologists Should Know, Radiographics, 1823-1842.
7. Koumbourlis, A. C. (2006) Scoliosis and the Respiratory System: Paediatric Respiratory Reviews, Elsevier, 7: 152 - 160.
8. Perkins, J., Boyer, A., Mcleish, A., Grossnickle, K. (2013) Idiopathic Scoliosis and Pelvic Floor Dysfunction, IJTR, 19; 2.
9. Romano, M. Negrini, A., Parzini, S., Tavernaro, M., Zaina, F., Donzelli, S., Negrini, S. (2015) SEAS (Scientific Exercises Approach to Scoliosis): a modern and effective evidence based approach to physiotherapy specific scoliosis exercises, Biomed Central, 10: 3.
10. Scoliosis Association UK https://www.sauk.org.uk/types-of-scoliosis/syndromic-scoliosis
11. Stitzel , C. (2017) The Different Scoliosis Locations & Types of Spinal, [ONLINE], Curvatures, https://www.treatingscoliosis.com/blog/scoliosis-spinal-curvature-types/
12. Uden, A., Nilsson, I. M., Willner, S. (1980) Collagen Changes In Congenital And Idiopathic Scoliosis , Acta Orthop. scand; 51: 271-274.